Equity and Best Practice immunisation

This factsheet covers equity and best practice principles, established during COVID-19 by the World Health Organisation (WHO). We believe these principles should guide all our work in immunisation.
Overview
WHO vaccination principles
During COVID the World Health Organisation (WHO) established the following principles, which we believe should guide all our work on immunisation:
- Equity: all individuals, populations and countries should have equitable vaccine access without incurring financial hardship
- Quality: the vaccines used should meet international standards through WHO authorization
- Integrated: vaccines should be deployed with tests, treatments, public health and social measures
- Inclusivity: vaccination must include marginalized, vulnerable, displaced, and imprisoned populations.
These are consistent with and additional to our commitment in Aotearoa New Zealand to te Tiriti o Waitangi in healthcare: providing Tino rangatiratanga, equity, active protection, options and partnership in all that we do.
Best practice immunisation requires us to address equity and clinical issues. We consider what are the barriers to people getting vaccinated, and how can we remove them, through to how to ensure immunisation is safe and effective, and that people understand what to look out for after they're vaccinated.
Lifting immunisation rates and equity
A patient journey
The following story depicts the experiences that many whānau have. We need to think about how we can deliver more appropriate and acceptable care that recognises the challenges families and individuals face.
When my baby turned 6 weeks old, I rang the GP to get an appointment for her immunisation. I had to ring 3 times to get through. When we finally got through, they said that we owed $20 on the account from some phone calls. I booked for the next week so I would have the money to pay.
On the day of the appointment my other kids had colds so they were home from school, even though it was not covid, you’re not allowed to bring your other children in to the doctor’s appointments, so we couldn’t go for her shots. So, I booked another appointment for the next week.
Next week my in-laws got sick, my father-in-law was in hospital and my husband needed the car that day to take him up to the hospital and help his mum, so we couldn’t get there. I tried to get my sister to take us, but she didn’t have a car-seat. I booked again for 10 days later, we were short on money that week as my husband had taken time off work, so we needed to wait to get money for petrol and fees we owed for the clinic
I finally got to take my baby to the doctors when she was 9 weeks old. We had to answer lots of question before we were even allowed in the door, but we’re getting used to that these days. I tried to keep her all wrapped up while waiting outside, and away from anyone else in the waiting room, someone in there was coughing, it’s scary these days with Covid around.
When I saw the nurse, she commented that we were overdue for the injections. She was new, we didn’t know each other, and she was in a rush, so I didn’t have a chance to explain, but I felt like she was saying that I was a bad mother. I asked her if the baby injections were the same as the ones my other kids had, she seemed to get annoyed and said it was up to me if I didn’t want them to get the injections. That wasn’t what I meant; I didn’t want to ask her anything else after that even though I would have liked another bottle of paracetamol. I used to feel more comfortable with the old nurse, she knew my whānau and we could have a nice chat.
I’m not sure if I can get my baby’s next injections at 3 months, or if I should get the next ones late since we were late for the 6-week-old ones. I might not be able to book an appointment; the receptionist asked me to fill in lots of forms and said I need to give them a copy of baby’s birth certificate, but I don’t have one yet. And I’ll be back at work by then - I can’t take a day off when I’ve just started back. Hopefully one of the whānau will be able to take them.
[The patient journey is reproduced with the permission of Dr Ranche Johnson (she/her), Clinical Director, Ngāpuhi]
Making whānau feel welcome
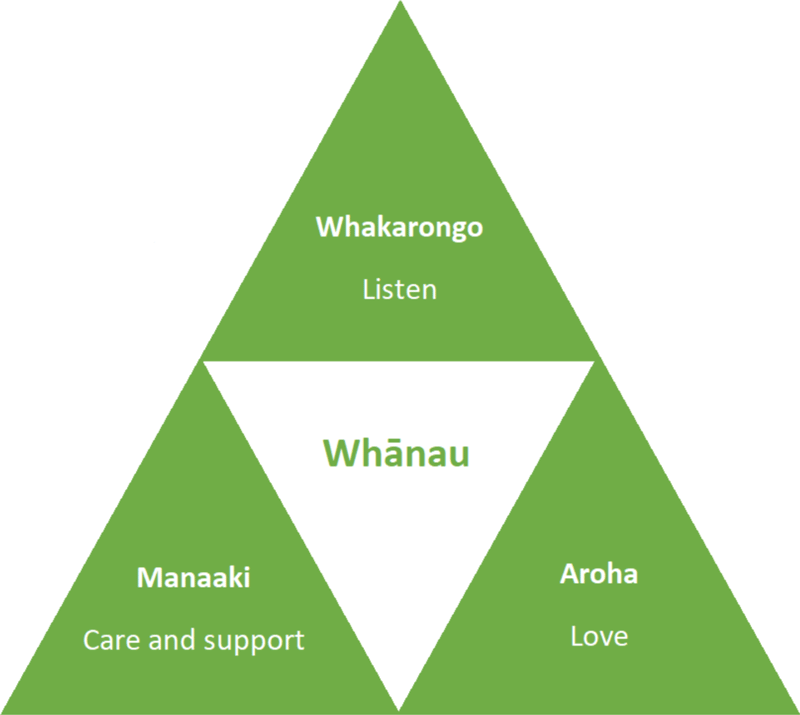
- Provide a positive, whānau centred environment providing manaakitanga, aroha and active listening approach to ensure the family feels welcome.
- Ensure your clinic communicates to whānau that you have prepared for them to ensure they have a safe and positive experience.
- Be flexible to unforeseen circumstances which occur.
- Have a play area for the children.
- Provide cultural awareness training for all staff and volunteers.
Tips to improve equity and child immunisation levels
Research shows that one strategy will not solely by itself improve childhood immunisation rates and highlights the importance of having a toolkit of strategies that you can utilise and adapt for your community.
We are always keen to hear about what strategies you are using that have been successful so we can add to our tips for others to trial.
Here are some options you can consider for your clinic or practice to follow.
Top ten tips
1. Have a practice or clinic Immunisation Champion.
2. Accept all newborn nomination messages daily.
3. Pre-call babies at 4 weeks of age. Welcome baby to practice, book appointment, offer enrolment. Phone to confirm appointment.
4. Consider barriers to access and offer support *(see below).
5. Offer opportunistic immunisation, all practice staff can use patient alerts or check recalls to identify attending patients who have overdue immunisation. Also immunise non-enrolled casual babies if the opportunity arises.
6. Do not postpone or cancel immunisation appointments for babies or other people who are mildly unwell.
7. Ensure your practice feels safe to whānau with precious babies.
- Consider offering immunisation in ‘green plus’ streams ie not co-mingling with winter illnesses.
- Consider separate clinic times for immunisation or ‘Well-child Saturdays’.
- Consider calling babies in from car to immunisation room, or immunising in cars.
8. Ensure your practice is welcoming to whānau. Whakawhanaungatanga is important.
- Engagement with whānau of newborn babies is an opportunity to build trusting relationships.
- First impressions count. Don’t focus on the invoice. “Kia ora” and a smile goes a long way.
- Ensure that whānau feel seen and heard and valued.
9. Prioritise immunisation recalls with an equity approach.
- Recall Māori and Pasifika and those whānau with high barriers to access first (eg those with disabilities, or from low socioeconomic areas).
- Consider dedicating staff to contact/phone these patients to discuss the importance and benefits of immunisation and to address any concerns or barriers.
- Ideally this would be a qualified member of staff who is matched from ethnicity and/ or language perspective.
10. Prompt referral to outreach services (OIS) if whānau have not been immunised after 3 recalls, 4 weeks overdue. Continue to recall whānau of children who have been referred to OIS.
*Addressing Barriers to access
Transport
Consider offering staff to transport whānau, using FFP, offering petrol vouchers, St Johns Shuttle, early referral to outreach.
Housing/ Mobility
Check contact details at every contact, get email details, next of kin contact.
Time
Offer immunisation out of working day eg, evening or weekend Well Child clinic.
Non-discrimination
Immunisation services need to be holistic and listen to the concerns of whānau; staff who look like the whānau they serve; staff trained in cultural safety and Māori models of care.
Cost
Immunisation offered completely free without any requirement for other accounts to be paid.
Enrolment
Babies are eligible to be enrolled if in the care and control of a parent/ legal guardian who is eligible to be enrolled – do not delay enrolment until a birth certificate is presented.
Other processes to improve immunisation rates
Overdue Immunisations:
- Each month your practice receives a report via email from the National Immunisation Register (NIR) team, used to identify overdue immunisations or missing vaccine data/messages
- These reports must be completed in full and returned to the NIR within two weeks and prompt action taken to recall patients identified as overdue for immunisation and/or to correct errors or missing NIR data.
Transfers/overseas:
- When the practice becomes aware that a child has transferred to another practice or has moved overseas (for more than two months) the NIR should be notified.
Authorised User Agreements:
- To ensure Immunisation messages get to NIR, please make sure all new staff/vaccinators have completed an AUA form and sent it to NIR. NIR publications – see forms at the bottom of the linked page.
Promotion and education:
- Promote immunisation with resources available in your practice, such as posters, pamphlets (including resources in te reo Māori and other languages) – available on the HealthEd website
- It is important to have conversations with families that decline or repeatedly delay immunisations to ensure that they have the opportunity to discuss their concerns and get good information from you.
Before you can vaccinate
Ensure vaccinator is an authorised/pharmacist vaccinator ie has:
- Completed an approved vaccinator training course
- Passed open book assessment & clinical assessment
- Pharmacists have advised PSNZ of vaccinator status
- Registered Nurses have received authorisation from medical officer of health
- Have current indemnity insurance
- Have current CPR certificate
- NB: Authorisation/pharmacist vaccinator status is valid for two years, from date of initial course. Individuals are responsible for re-application after approved vaccinator update course, two yearly.
Ensure the emergency kit is ready to use with:
- Adrenaline 1:1000 (min 3 ampoules) and dosage chart
- Syringes: 1.0mL (minimum of 6 tuberculin syringes)
- Needles: a range of needle lengths and gauges, including 23G or 25G x 25mm, 22G x 38mm
- Adult and paediatric bag valve mask resuscitator (eg ambu bag), oxygen tubing and a range of oxygen masks
- Access to a telephone.
NB: A second person must be onsite at the time of vaccination and for at least 20 minutes post vaccination
NB: It is acceptable to wait for the ambulance to bring oxygen and airway equipment in settings where they are not needed for other emergencies.
Assemble the quick needles
*Consideration may be given to the vastus lateralis as an alternative vaccination site, providing it is not contraindicated.
Just before vaccinating
Pre-vaccination checklist
- Run a “status query” via the PMS prn
- Obtain consent for the vaccination event, and for the information to be held on the NIR
- Advise of 20 min wait following the immunisation.
Prior to immunisation, check if the vaccinee:
- is unwell on that day, has a fever (if concerned, check temperature) or has any new diagnosis/medications
- has ever had a serious reaction to any vaccine
- has any severe allergies to vaccine components (e.g. gelatin, egg protein, yeast, neomycin)
- has appropriate spacing between doses of the same vaccine (when was the last vaccination?)
- is pregnant or planning pregnancy
- has an undiagnosed/evolving neurological condition (pertussis containing vaccine only)
- is/has been treated with immune suppressing medication.
Additional precautions to check prior to immunisation with a live vaccine, check if the vaccinee:
- has lowered immunity/is on immunosuppressive drugs
- if child’s mother has been on immune suppressing medication during pregnancy
- has had any live vaccines in the last four weeks
- has had an injection of immunoglobulin or blood
Just after vaccination
Collect vaccination information
Record details in the Well Child Tamariki Ora book (WCTO); vaccines given, injection site, and route used.
Record the following information in the PMS:
- vaccines given (dose and series), injection sites, route, needle length and gauge
- informed consent obtained (including . from who)
- AIR consent (vaccines given recorded on the NIR)
- that the vaccinee was well
- any known allergies or contraindications
- that they were advised to wait 20 mins
- details of any adverse event(s) following immunisation
Provide post-vaccination advice
- Advice needs to be given verbally and in writing
- Discuss expected responses and what to do
- Discuss when to contact the vaccinator or after hours medical service if worried/concerned
- Provide immunisation information and after hours contact number (eg Aftercare sheet HE1504 or resource appropriate for that immunisation event)
- Check the injection site prior to the vaccinee leaving.
CALL 0800 IMMUNE (466 863) for clinical advice





